◊Youth Traumatic Stress Smart Services ◊
Youth Traumatic Stress Smart Services (YTSSS) is a Category lll National Child Traumatic Stress Initiative (NCTSI) housed at the Olive View UCLA Medical Center. Funded by the Substance Abuse and Mental Health Services Adminisatration (SAMHSA)in 2021, the goal of YTSSS is to provide grief-enhanced trauma-informed evaluation and management to at-risk youth and their caregivers in North Los Angeles County. The YTSSS team focuses its work on providing such services at pediatric primary and specialty care, HUB clinics, Juvenile Justice, Regional Center, Los Angeles Unified School District, Veteran Affairs (VA) and military family clinics, and emergency room settings.
The United States is currently facing a profound public crisis of traumatic stress and grief, affecting millions of youth and families across the country. Los Angeles, as one of the most populous and diverse cities, is significantly impacted by this crisis. Trauma and grief stem from various sources, including the COVID-19 pandemic, social injustices, violence, and natural disasters. The impact of these events on mental health is profound, necessitating an urgent response from both the public and mental health professionals.
Trauma and Grief: A Nationwide Perspective
According to SAMHSA, approximately 70% of adults in the United States have experienced some type of traumatic event at least once in their lives. The COVID-19 pandemic has exacerbated these issues, with increased rates of anxiety, depression, and posttraumatic stress disorder (PTSD) reported across the nation. In 2022, the Centers for Disease Control and Prevention (CDC) reported that over 40% of adults experienced symptoms of anxiety or depressive disorder during the pandemic.
The Impact on Los Angeles
Los Angeles has been particularly affected due to its large population and its unique challenges. Data from the Los Angeles County Department of Public Health reveals that the city has seen a significant rise in mental health issues. In 2021, 1 in 4 adults in Los Angeles County reported needing mental health services, a notable increase from previous years. Additionally, the city has faced numerous challenges, including homelessness, racial tensions, and economic disparities, all contributing to the mental health crisis. The recent wildfires in Los Angeles in 2025 have caused significant trauma, leading to increased rates of anxiety, depression, and potentially PTSD among residents, first responders, and vulnerable populations. Increased access to grief-enhanced trauma-informed care, social support, and resilience-building programs will help affected individuals recover.
Youth Traumatic Stress Smart Services (YTSSS) is a Category lll National Child Traumatic Stress Initiative (NCTSI) housed at the Olive View UCLA Medical Center. Funded by the Substance Abuse and Mental Health Services Administration (SAMHSA)in 2021, the goal of YTSSS is to provide grief-enhanced trauma-informed evaluation and management to at-risk youth and their caregivers in North Los Angeles County. The YTSSS team focuses its work on providing such services at pediatric primary and specialty care, HUB clinics, Juvenile Justice, Regional Center, Los Angeles Unified School District, Veteran Affairs (VA) and military family clinics, and emergency room settings.
The United States is currently facing a profound public crisis of traumatic stress and grief, affecting millions of youth and families across the country. Los Angeles, as one of the most populous and diverse cities, is significantly impacted by this crisis. Trauma and grief stem from various sources, including the COVID-19 pandemic, social injustices, violence, and natural disasters. The impact of these events on mental health is profound, necessitating an urgent response from both the public and mental health professionals.
Trauma and Grief: A Nationwide Perspective
According to SAMHSA, approximately 70% of adults in the United States have experienced some type of traumatic event at least once in their lives. The COVID-19 pandemic has exacerbated these issues, with increased rates of anxiety, depression, and posttraumatic stress disorder (PTSD) reported across the nation. In 2022, the Centers for Disease Control and Prevention (CDC) reported that over 40% of adults experienced symptoms of anxiety or depressive disorder during the pandemic.
The Impact on Los Angeles
Los Angeles has been particularly affected due to its large population and its unique challenges. Data from the Los Angeles County Department of Public Health reveals that the city has seen a significant rise in mental health issues. In 2021, 1 in 4 adults in Los Angeles County reported needing mental health services, a notable increase from previous years. Additionally, the city has faced numerous challenges, including homelessness, racial tensions, and economic disparities, all contributing to the mental health crisis. The recent wildfires in Los Angeles in 2025 have caused significant trauma, leading to increased rates of anxiety, depression, and potentially PTSD among residents, first responders, and vulnerable populations. Increased access to grief-enhanced trauma-informed care, social support, and resilience-building programs will help affected individuals recover.
OUR MISSION is to improve the quality of care and make it easier for traumatized children, their families, and communities across the United States to get the support they need and the appropriate level of care.
OUR MISSION is to improve the quality of care and make it easier for traumatized children, their families, and communities across the United States to get the support they need and the appropriate level of care.
High Prevalence
Up to 80% of children experience at least one significant potential traumatic stress exposure (PTE) in childhood. Up to 80% of children experience at least one significant potential traumatic stress exposure (PTE) in childhood. Posttraumatic stress disorder (PTSD) is common in north Los Angeles County (LAC), where the majority of them receiving services are children (51.5%), which is disproportionately higher amongst minority ethnic groups, children of military and Veteran families as well as those involved in Juvenile Hall. Childhood bereavement is common in North LAC, especially in minority ethnic groups. An increased prevalence of children with PTSD and associated suicidality who visited the psychiatry emergency room (PER) at Olive View UCLA Medical Center was noted, especially COVID-19-related PTSD and grief.
Poor Mental Health Outcomes
After exposure to traumatic and loss experiences, some children and adolescents develop adverse traumatic stress responses, including Acute Stress Disorder (ASD), Posttraumatic Stress Disorder (PTSD), or prolonged grief disorder. They are also at risk for suicidal and homicidal intent and other mental health comorbidities. In addition, the risk of developing traumatic stress disorder is significantly higher in those with comorbid attention deficit hyperactive disorder (ADHD), autism spectrum disorder, etc. Poor health outcomes and lower life expectancy. PTSD and Bereavement are associated with increased aggressive behavior and, emotional constriction, social withdrawal. PTSD and Bereavement are related to impaired cardiovascular function, sleep disturbances, increased neuroinflammation, suicidality, and significant adverse health events.
High Cost
Childhood PTSD is a significant public health problem with serious health consequences to children and a financial burden to society, with an estimated cost of $103 billion annually.
Often Underdiagnosed and Misdiagnosed
The lack of scalable early screening for high-risk behaviors related to PTSD and the absence of early identification and risk stratification based on such behaviors resulted in many individuals with PTSD going undiagnosed and not receiving early interventions.
Early Identification and Integrated Care Using Evidence-Based Treatments is Associated with Positive Outcomes
Grief-enhanced trauma-informed interventions are associated with reduction of the severity of core PTSD and grief symptoms and improve neuropsychiatric functioning among children with PTSD and parental/caregiver functioning, and positive outcomes. They are associated with higher adjustment levels and enhanced parent/caregiver-child interactions.
Using the Grief-enhanced Trauma-informed Care Process Model
Youth 9 years and older, will receive evaluation of traumatic stress symptoms, bereavement symptoms, protective factors measurement, functional level and wellbeing assessments. Those with a potentially traumatic stress/ loss experience(s), the process of responding effectively to child traumatic stress/loss involves three steps:
1. Report if required.
In Los Angeles, reports can be made to either local law enforcement or to the Department of Child Protective Services (1-800-540-4000).
2.Respond to suicide risk.
If the parent or youth endorses any number of days of suicidal thinking, youth and caregivers will receive the digital message(s) on suicide safety planning, crisis management information, and suicide hotlines, also, mental health clinicians will evaluate the youth to determine severity of risk and appropriate response.
3. Stratify treatment approach.
Results and responses from the Grief-enhanced Trauma-informed Evaluation are stratified into 4 levels. No symptoms with traumatic stress prevention preparation, mild symptoms with protective approach to enhance coping skills, the moderate symptoms with age-appropriate resilient approach of grief-enhanced trauma-informed interventions, and the severe symptoms with restorative approach of crisis stabilization and grief-enhanced trauma-informed psychotherapy and psychotropic med management, if needed.
Using Positive Biopsychosocial Profile (PBP)
The experience of trauma and grief can vary significantly from one individual to another, influenced by a range of vulnerability and protective factors that either exacerbate or mitigate the severity of symptoms for youth and caregivers. This comprehensive approach ensures that our evaluations are thorough and scientifically grounded, facilitating effective treatment strategies for individuals suffering from trauma and grief.
Using the Grief-enhanced Trauma-informed Interventions (GTI)
Youth with potential traumatic stress/loss exposures (PTE) can receive a tailored intervention based on the symptom severity, functional impairment and wellbeing status. This includes referrals to brief interventions, mental health professionals, support groups, and other resources that offer preventive and curative interventions. For those without symptoms, our program offers disaster and traumatic stress preparedness and preventive psychoeducational trainings to prepare them for potential future trauma and stressors. These programs focus on building resilience, enhancing coping mechanisms, and providing mental health and well-being knowledge. For those with mild to severe symptoms based on the functional levels and wellbeing impairment, brief in-office grief-enhanced trauma-informed interventions targeting the core symptoms will be provided. For those with suicidality and traumatic stress and/or Bereavement the, grief-enhanced trauma-informed emergency room services will be offered.
Follow up at regular intervals
Youth at risk for traumatic stress and bereavement will be evaluated on regular basis to assess the change in symptoms, functional level, and wellbeing in response to grief-enhanced trauma-informed services.
The Grief Trauma Team is a multi-disciplinary team including faculty and providers from the University of California Los Angeles, Los Angeles County Department of Health Services, and Department of Mental Health and other programs. We also collaborate with providers and faculty from other institutions and settings.
High Prevalence
Up to 80% of children experience at least one significant potential traumatic stress exposure (PTE) in childhood. Up to 80% of children experience at least one significant potential traumatic stress exposure (PTE) in childhood. Posttraumatic stress disorder (PTSD) is common in north Los Angeles County (LAC), where the majority of them receiving services are children (51.5%), which is disproportionately higher amongst minority ethnic groups, children of military and Veteran families as well as those involved in Juvenile Hall. Childhood bereavement is common in North LAC, especially in minority ethnic groups. An increased prevalence of children with PTSD and associated suicidality who visited the psychiatry emergency room (PER) at Olive View UCLA Medical Center was noted, especially COVID-19-related PTSD and grief.
Poor Mental Health Outcomes
After exposure to traumatic and loss experiences, some children and adolescents develop adverse traumatic stress responses, including Acute Stress Disorder (ASD), Posttraumatic Stress Disorder (PTSD), or prolonged grief disorder. They are also at risk for suicidal and homicidal intent and other mental health comorbidities. In addition, the risk of developing traumatic stress disorder is significantly higher in those with comorbid attention deficit hyperactive disorder (ADHD), autism spectrum disorder, etc. Poor health outcomes and lower life expectancy. PTSD and Bereavement are associated with increased aggressive behavior and, emotional constriction, social withdrawal. PTSD and Bereavement are related to impaired cardiovascular function, sleep disturbances, increased neuroinflammation, suicidality, and significant adverse health events.
High Cost
Childhood PTSD is a significant public health problem with serious health consequences to children and a financial burden to society, with an estimated cost of $103 billion annually.
Often Underdiagnosed and Misdiagnosed
The lack of scalable early screening for high-risk behaviors related to PTSD and the absence of early identification and risk stratification based on such behaviors resulted in many individuals with PTSD going undiagnosed and not receiving early interventions.
Early Identification and Integrated Care Using Evidence-Based Treatments is Associated with Positive Outcomes
Grief-enhanced trauma-informed interventions are associated with reduction of the severity of core PTSD and grief symptoms and improve neuropsychiatric functioning among children with PTSD and parental/caregiver functioning, and positive outcomes. They are associated with higher adjustment levels and enhanced parent/caregiver-child interactions.
Using the Grief-enhanced Trauma-informed Care Process Model
Youth 9 years and older, will receive evaluation of traumatic stress symptoms, bereavement symptoms, protective factors measurement, functional level and wellbeing assessments. Those with a potentially traumatic stress/ loss experience(s), the process of responding effectively to child traumatic stress/loss involves three steps:
1. Report if required.
In Los Angeles, reports can be made to either local law enforcement or to the Department of Child Protective Services (1-800-540-4000).
2.Respond to suicide risk.
If the parent or youth endorses any number of days of suicidal thinking, youth and caregivers will receive the digital message(s) on suicide safety planning, crisis management information, and suicide hotlines, also, mental health clinicians will evaluate the youth to determine severity of risk and appropriate response.
3. Stratify treatment approach.
Results and responses from the Grief-enhanced Trauma-informed Evaluation are stratified into 4 levels. No symptoms with traumatic stress prevention preparation, mild symptoms with protective approach to enhance coping skills, the moderate symptoms with age-appropriate resilient approach of grief-enhanced trauma-informed interventions, and the severe symptoms with restorative approach of crisis stabilization and grief-enhanced trauma-informed psychotherapy and psychotropic med management, if needed.
Using Positive Biopsychosocial Profile (PBP)
The experience of trauma and grief can vary significantly from one individual to another, influenced by a range of vulnerability and protective factors that either exacerbate or mitigate the severity of symptoms for youth and caregivers. This comprehensive approach ensures that our evaluations are thorough and scientifically grounded, facilitating effective treatment strategies for individuals suffering from trauma and grief.
Using the Grief-enhanced Trauma-informed Interventions (GTI)
Youth with potential traumatic stress/loss exposures (PTE) can receive a tailored intervention based on the symptom severity, functional impairment and wellbeing status. This includes referrals to brief interventions, mental health professionals, support groups, and other resources that offer preventive and curative interventions. For those without symptoms, our program offers disaster and traumatic stress preparedness and preventive psychoeducational trainings to prepare them for potential future trauma and stressors. These programs focus on building resilience, enhancing coping mechanisms, and providing mental health and well-being knowledge. For those with mild to severe symptoms based on the functional levels and wellbeing impairment, brief in-office grief-enhanced trauma-informed interventions targeting the core symptoms will be provided. For those with suicidality and traumatic stress and/or Bereavement the, grief-enhanced trauma-informed emergency room services will be offered.
Follow up at regular intervals
Youth at risk for traumatic stress and bereavement will be evaluated on regular basis to assess the change in symptoms, functional level, and wellbeing in response to grief-enhanced trauma-informed services.
The detailed resources can be found in the list of menus and submenus for evaluation and management of youth at risk of traumatic stress disorder and bereavement.
The Grief Trauma Team is a multi-disciplinary team including faculty and providers from the University of California Los Angeles, Los Angeles County Department of Health Services, and Department of Mental Health and other programs. We also collaborate with providers and faculty from other institutions and settings.
YTSSS Partnerships





YTSS Partnerships





Other Markers For Traumatic Stress And Grief- Vascular Markers
Traumatic stress and grief are not only psychological phenomena but also involve profound physiological changes, particularly within the cardiovascular and vascular systems. Dysregulation of vascular markers is a key aspect of the psychophysiological response, driven by the interaction between the nervous, endocrine, and immune systems.
Other Markers For Traumatic Stress And Grief- Sleep Disturbances
Traumatic stress disorder (e.g., PTSD) is often characterized by sleep disturbances, including insomnia, nightmares, and fragmented sleep. Actigraphy, polysomnography (PSG), Electroencephalography (EEG) and event-related potentials (ERPs) are critical tools for identifying neurophysiological alterations underlying these disturbances.
Other Markers For Traumatic Stress And Grief- Vascular Markers
Traumatic stress and grief are not only psychological phenomena but also involve profound physiological changes, particularly within the cardiovascular and vascular systems. Dysregulation of vascular markers is a key aspect of the psychophysiological response, driven by the interaction between the nervous, endocrine, and immune systems.
Other Markers For Traumatic Stress And Grief- Sleep Disturbances
Traumatic stress disorder (e.g., PTSD) is often characterized by sleep disturbances, including insomnia, nightmares, and fragmented sleep. Actigraphy, polysomnography (PSG), Electroencephalography (EEG) and event-related potentials (ERPs) are critical tools for identifying neurophysiological alterations underlying these disturbances.
Collaboration
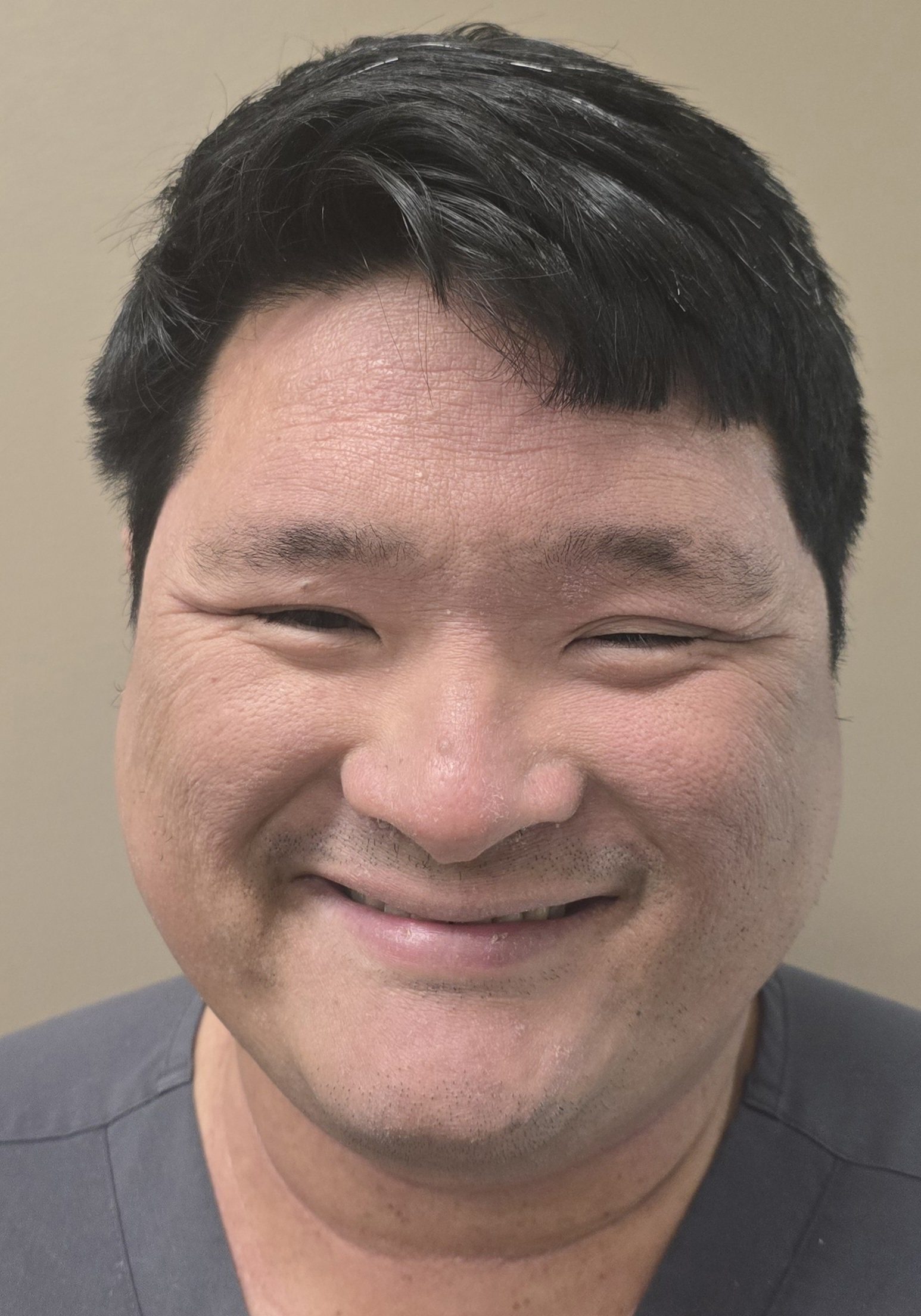
Joseph Rojas MD
Shanica Davis NP
Gilberto Bultron MD
Shannon Thyne MD
Consultants
Alan Steinberg PhD
Brooks Keeshin MD
Joan Asarnow PhD
Gregory Leskin PhD