LEVEL OF CARELEVEL OF CARE
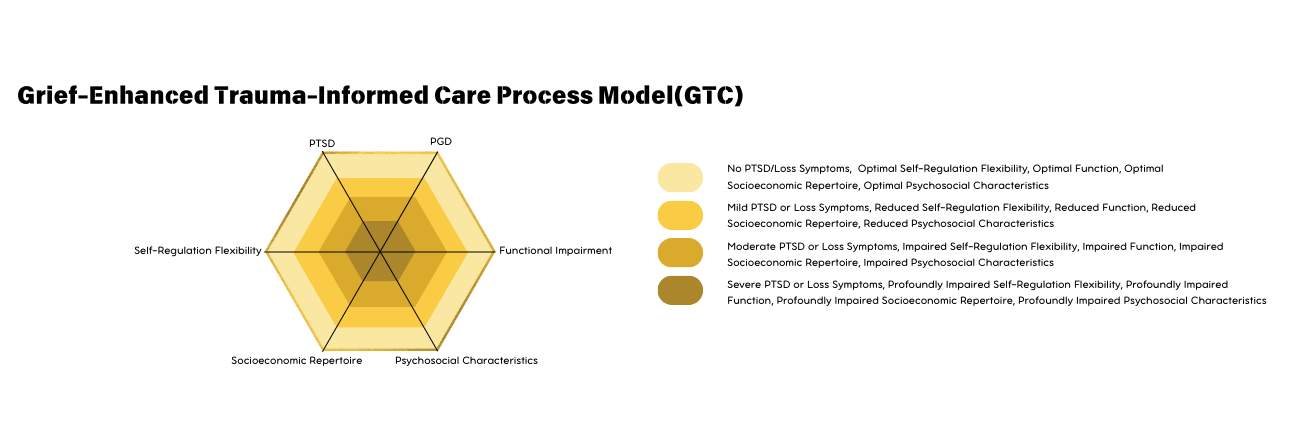
Hexagon Diagram For Levels Of Care
Our Grief-Enhanced Trauma-Informed Care Process Model differs from the traditional psychiatry approach that focuses on the presence and severity of mental illness. In our model, we evaluate the mental wellbeing, self and social engagement, and optimal functioning and socioeconomic repertoire in addition to the severity of psychiatric symptoms.
Our model facilitates:
a) Understanding underlying psychological, physiological, and environmental protective and vulnerability factors related to traumatic stress symptoms.
b) Enhancing an individual’s functioning by promoting self-regulation flexibility and positive biopsychosocial characteristics for their thriving.
c) Stratifying for preventive measures and treatment based on scalable, quantitative measures of severity of traumatic stress/loss symptoms and their related psychosomatic symptoms.
d) Monitoring the response and outcome of individuals to grief-enhanced trauma-informed interventions.



Severity of PTSD (post traumatic stress disorder)
PTSD severity depends on how intense, frequent, and lasting its symptoms are, affecting emotional regulation, daily life, and relationships. Severe symptoms can lead to anxiety, mood swings, and emotional numbness, making it hard to function at work, school, or in social settings. The brain stays in a heightened stress state, causing chronic distress and making it difficult to feel safe or find joy. Without treatment, PTSD can lead to long-term mental and physical health issues, such as depression and substance use.

Total score /8
Reactivity to Trauma Reminders
Individuals with PTSD may experience intense emotional or physiological reactions when exposed to reminders of their trauma. This hyper-reactivity can trigger panic, fear, or distress, making daily life unpredictable and stressful. Over time, this can lead to avoidance behaviors, limiting one’s ability to engage in normal activities.
Trauma Hypervigilant Intrusive Thoughts
PTSD often involves intrusive, unwanted thoughts about the traumatic event. These thoughts can manifest as flashbacks, nightmares, or distressing mental images. Hypervigilance—a heightened state of alertness—can cause difficulty relaxing, sleeping, and focusing, leading to chronic stress and exhaustion.
Trauma Avoidance Negative Affectivity
Avoidance behaviors emerge as individuals try to suppress trauma-related emotions, places, or people associated with their distress. However, this avoidance can reinforce fear and limit engagement in meaningful experiences. Negative affectivity, such as persistent sadness, anger, or emotional numbness, contributes to difficulties in maintaining relationships and overall well-being.
Trauma Sleep Problems
PTSD often disrupts sleep through nightmares, insomnia, or restless sleep. Sleep deprivation worsens emotional regulation, cognitive function, and overall resilience, creating a cycle of heightened distress and reduced coping ability.
Severity of PGD (Prolonged grief Disorder)
Prolonged Grief Disorder (PGD) is a persistent and debilitating form of grief that disrupts daily life. Unlike typical grief, which lessens over time, PGD is marked by prolonged sorrow, emotional pain, and an intense preoccupation with the deceased. Individuals often struggle to accept their loss, experiencing deep emptiness and disconnection. This can impair cognitive function, social relationships, and physical health, leading to issues like fatigue, weakened immunity, and stress-related conditions. Feelings of guilt, regret, and a loss of purpose further intensify emotional distress. Without proper support, PGD can result in severe mental health challenges, making early intervention essential for recovery.

Total Score: /8
Reactivity to Loss Reminders
Similar to PTSD, PGD involves strong emotional responses to reminders of the deceased. These reactions can include profound sadness, longing, or distress, often making it difficult for individuals to engage in daily activities without experiencing emotional breakdowns.
Loss Separation distress
This symptom refers to intense longing for the deceased, persistent feelings of emptiness, and difficulty accepting the reality of loss. It can lead to social withdrawal, depression, and an inability to find joy in life without the lost loved one.
Loss Existential Distress
Individuals with PGD often struggle with existential concerns, questioning the meaning of life and their purpose after the loss. Feelings of hopelessness, identity confusion, and a sense of being lost can make it difficult to re-engage with life and relationships.
Loss Circumstantial distress
Some individuals experience distress linked to the specific circumstances of the loss (e.g., a sudden or traumatic death). This distress can intensify feelings of guilt, regret, or helplessness, making it harder to process grief and move forward.
Self-Regulation Flexibility (social wellbeing)
Self-regulation flexibility refers to an individual’s ability to manage and adapt their emotional, cognitive, and behavioral responses to trauma and grief. This ability is essential for mental resilience and long-term recovery. Self-regulation flexibility is crucial because it provides individuals with the psychological tools to cope with distress, maintain stability, and continue personal growth even after experiencing loss or trauma.

Total Score: /8 (Reversed)
Resilience
The capacity to bounce back from adversity, trauma, or loss. It helps individuals maintain mental stability despite experiencing distress. A lack of resilience can lead to prolonged emotional suffering, while strong resilience promotes quicker recovery and adaptability.
PERMA-V (Positive Emotions, Engagement, Relationships, Meaning, Achievement, and Vitality)
This model provides a framework for psychological well-being and growth. It encourages individuals to use multiple coping strategies such as finding meaning in loss, maintaining healthy relationships, and engaging in fulfilling activities. These strategies can help reduce hypervigilance and intrusive thoughts related to trauma.
Self-compassion, Gratitude (responsiveness to feedback)
Allows individuals to treat themselves with kindness and patience during the healing process. Gratitude fosters positive emotional states that counterbalance negative affectivity, helping individuals process trauma and grief in a more adaptive way.
Strength and Grit
Strength and grit refer to perseverance and determination when faced with hardship. Individuals who cultivate these traits can navigate distressing emotions, work through sleep disturbances, and remain functional in their daily lives despite grief or trauma
Functional Impairment (functional level)
Functional impairment refers to how trauma and grief affect an individual’s ability to perform daily activities and maintain relationships. This category focuses on the extent to which mental health struggles interfere with normal life functions. Addressing functional impairment is essential to maintaining overall well-being, as disruptions in daily life can exacerbate mental health struggles. Providing the right support can help individuals regain stability and reintegrate into their daily routines.

Total Score: /8
Self
Resilience The capacity to bounce back from adversity, trauma, or loss. It helps individuals maintain mental stability despite experiencing distress. A lack of resilience can lead to prolonged emotional suffering, while strong resilience promotes quicker recovery and adaptability.
Home, 1st degree
The effects of trauma and grief extend to immediate family and close relationships. Hypervigilance, intrusive thoughts, and emotional instability can cause tension in the home environment. This can lead to withdrawal, conflict, or difficulty maintaining supportive relationships.
Peer, friends, extended family
Trauma avoidance and negative affectivity can lead individuals to isolate themselves from friends and extended family. The loss of these social connections can create a cycle of loneliness and emotional distress, worsening the impact of trauma and grief.
Work/School
Sleep disturbances, emotional exhaustion, and cognitive difficulties caused by trauma and grief can impact performance in professional or academic settings. Individuals may struggle with concentration, deadlines, and interactions with colleagues or peers, leading to further stress and potential financial insecurity.
Psychosocial Characteristics (social interaction)
Psychosocial characteristics refer to the social and emotional traits that influence an individual’s ability to navigate trauma and grief. These characteristics impact interpersonal relationships, emotional resilience, and overall mental well-being. They determine how well an individual can maintain relationships and find support during difficult times. Cultivating these traits enhances mental resilience and provides a foundation for emotional healing.

Total Score: /8 (Reversed)
Acceptance
The ability to acknowledge trauma and grief without excessive resistance. It plays a crucial role in healing, as those who struggle with acceptance may experience prolonged distress, denial, and difficulty moving forward. Developing acceptance allows individuals to process emotions in a healthier way.
Conflict resolution
Trauma and grief can strain relationships, leading to misunderstandings, frustration, and avoidance of difficult conversations. Conflict resolution skills help individuals communicate effectively, rebuild trust, and maintain meaningful connections with loved ones. This extend beyond conflict with others and includes intrapersonal conflict and issues and dealing with the emotions that arise from them.
Commitment
Commitment refers to the willingness to engage with relationships, responsibilities, and personal growth despite experiencing distress. A strong sense of commitment can help individuals stay connected with their support networks, reinforcing their resilience.
High-quality connectedness
A sense of belonging and support is vital for mental health. Strong social connections reduce the risk of prolonged grief disorder (PGD) and post-traumatic stress disorder (PTSD) by providing emotional validation, encouragement, and a sense of purpose.
Socioeconomic Repertoire (care and support system)
Socioeconomic factors play a major role in determining access to mental health resources and overall well-being. A strong socioeconomic support system can mitigate the negative effects of trauma and grief, while limited resources can exacerbate distress. Socioeconomic factors directly impact mental health by determining the level of support and resources available. Ensuring equitable access to care and stable support systems is key to promoting resilience and recovery from trauma and grief.

Total Score: /8 (Reversed Except Access Limitation)
Access to care
Access to mental health services, including therapy, medication, and support groups, is crucial for trauma recovery. Individuals with limited access to care may struggle with untreated PTSD or PGD, leading to prolonged suffering.
Access limitation
Barriers to care, such as financial constraints, geographical location, or cultural stigma, can prevent individuals from seeking or receiving help. These limitations increase the likelihood of chronic mental health issues.
System of care in place
A structured system of support, including mental health professionals, family, and community resources, can provide individuals with the necessary tools to cope with trauma and grief. This system ensures they receive the help they need without facing unnecessary obstacles.
System of care in place
Beyond basic care, having a long-term support system that promotes growth and stability helps individuals move beyond survival and into a thriving state. This includes stable housing, employment opportunities, and social integration, all of which contribute to sustained well-being.